A triple punch gene therapy has cleared its first safety test in humans as it gives human stem cells three ways to defy HIV.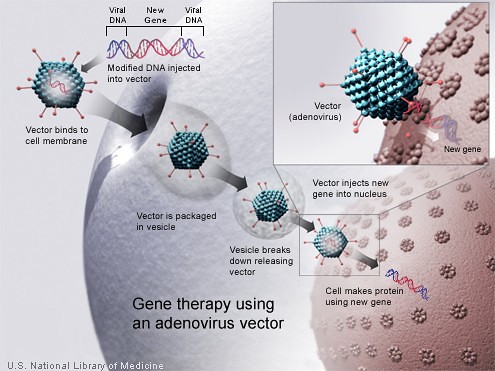
Four AIDS patients were injected with these cells and they tolerated the treatment and for up to two years, the cells produced anti HIV weapons.
Researchers are optimistic that after further clinical trials, combination therapy can replace or complement anti-retroviral drugs for treatment of HIV patients.
The trial piggybacked on a standard treatment where AIDS patients were given transplants of their previously saved blood stem cells for prevention of development of blood cancer. Besides normal blood stem cells, patients were also injected with cells in which three types of RNA based gene therapies were carried by a lentivirus. In the present trial, researchers combined genetic resistance into stem cells for replacing an immune system susceptible to HIV with one which can resist attack of the virus.
A triple-punch gene therapy, which endows human stem cells with three ways to resist HIV, has successfully cleared its first safety test in humans.
Four patients with AIDS who were infused with these cells tolerated the treatment, and the cells produced their anti-HIV weapons for up to two years.
While not many cells were transplanted in the trial to cure the patients or even reduce their viral load, researchers are hopeful that after further clinical trials, combination gene therapy may replace or complement anti-retroviral drugs as a way to treat people living with HIV.
The trial piggybacked on a standard treatment, in which individuals with AIDS receive transplants of their own previously saved blood stem cells, in an attempt to prevent the development of lymphoma (blood cancer).
In addition to normal blood stem cells, the patients were also given cells into which three types of RNA-based gene therapies were carried by a lentivirus.
In the current trial, the researchers engineered a combination of genetic resistance into stem cells, aiming to replace an immune system susceptible to HIV with one able to resist the virus’s attack.
Firstly, to stop HIV from penetrating the host cells, the researchers gave the cells an RNA enzyme that would cleave the message that codes for a protein called CCR5, preventing HIV from using the protein as a co-receptor to enter the cell.
"We know from a lot of populations that this is a great target — it can downregulate (HIV levels) by 90 per cent," Nature quoted John Rossi, a molecular biologist at the Beckman Research Institute of the City of Hope in Duarte, California, who worked on the trial, as saying.
But interfering with CCR5 is not foolproof, because HIV can evolve other ways of penetrating the cell.
"If somehow the virus should get into these cells, then we have the cells armed with two different approaches" to fight back, explained Rossi.
So the researchers used a second mode of attack, and inserted a decoy RNA that interferes with a viral protein called tat, which is important for replication.
Third, they used a technique called RNA interference (RNAi), in which they deployed a short sequence of RNA to degrade the message coding for that same viral protein and one of its partners in crime.
Such different mechanisms will make it harder for viral resistance to develop, noted Rossi.
In three of the four patients, the blood stem cells continued to produce these RNAs 18–24 months after they had received the transplant. The patients also showed no adverse reactions to the vector — a long-standing concern with gene therapy.
"It’s a small study, but it’s a step in the right direction. The most promising thing is that it shows you can modify stem cells in a way that makes them (HIV-)resistant, and the progeny of those cells would still be resistant to HIV and would still be functional," said Pablo Tebas, a clinical researcher at the University of Pennsylvania in Philadelphia who works on gene therapy and vaccines for HIV.
The study has been published in Science Translational Medicine.

0 comments:
Post a Comment